No Surprises Act: Financial Implications for Laboratory Services/Pathology
-
April 14, 2022
DownloadsDownload Article
-
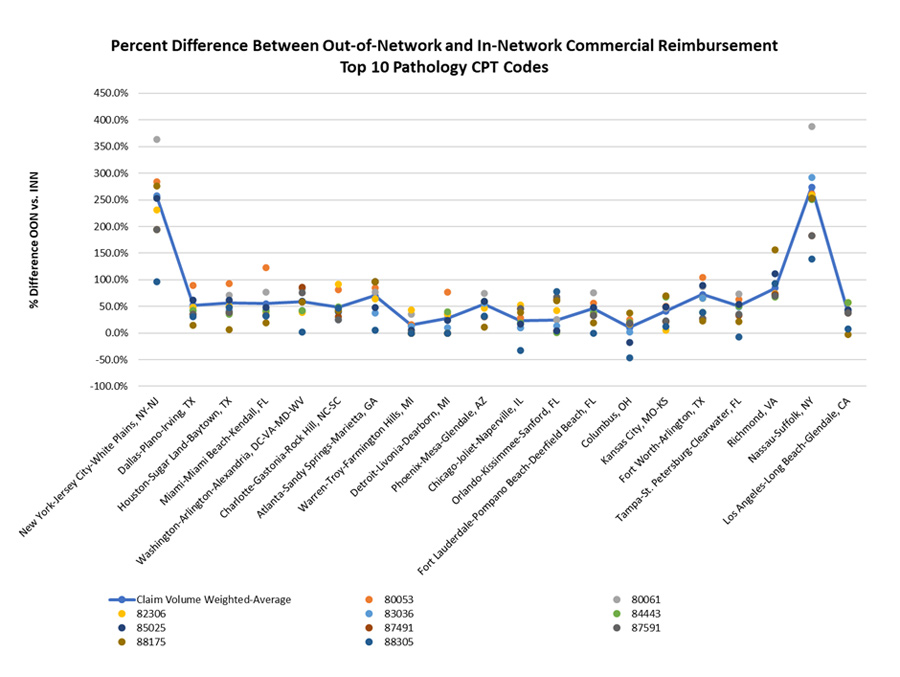
In this article, we explore the financial implications to laboratory services/pathology departments in 20 of the largest metropolitan statistical areas (MSAs).
FTI Consulting completed a pricing analysis of 10 common laboratory services/pathology Current Procedural Terminology (CPT) codes using IBM Watson’s MarketScan Commercial Claims and Encounters Database accounting for 35% of outpatient claims.
What You Need to Know
The No Surprises Act (NSA) became effective January 1, 20221. The American Hospital Association summarized the NSA’s main provisions as:
- “Protects patients from receiving surprise medical bills resulting from gaps in coverage for emergency services and certain services provided by out-of-network clinicians at in-network facilities, including by air ambulances.
- Holds patients liable only for their in-network cost-sharing amount, while giving providers and insurers an opportunity to negotiate reimbursement.
- Allows providers and insurers to access an independent dispute resolution process in the event disputes arise around reimbursement.
- Requires both providers and health plans to assist patients in accessing health care cost information2.”
Ancillary services such as pathology and laboratory services are always subject to balance billing provisions of the No Surprises Act. Services “don’t need to happen physically within the in-network health care facility to be treated as part of a visit3.” Notice and consent exceptions do not apply to non-emergency ancillary services such as pathology and laboratory services4. The No Surprises Act does not regulate non-emergency services provided in an out-of-network hospital, outpatient hospital department or ambulatory surgical center5.
| CPT Code | Description |
| 80053 | Comprehensive metabolic panel |
| 80061 | Lipid panel |
| 82306 | Vitamin D assay |
| 83036 | Glycosylated hemoglobin |
| 84443 | Thyroid stimulating hormone |
| 85025 | Complete blood count |
| 87491 | Chlamydia, Gonorrhea |
| 87591 | Infectious disease detection by nucleic acid |
| 88175 | Cytopathology, cervical or vaginal (Pap smear) |
| 88305 | Surgical pathology, gross and microscopic exam |
All Healthcare Is Local
FTI Consulting analyzed laboratory medicine/pathology claims data from the 20 largest MSAs. In-network claims accounted for 98.7% of the sample; out-of-network were 1.3%. These figures are substantially below the literature reporting out-of-network surprise bills of 12.9%, a figure surpassed only by emergency departments with 16.5%.6 The literature included only in-network facilities such as hospitals, hospital outpatient departments and emergency centers as the point of laboratory medicine/pathology origination, whereas our sample includes community origination; the number of out-of-network claims in the latter is far lower.
On a weighted average basis (across MSAs), the median in-network test ranges in price from $7.93 for a comprehensive metabolic panel (CPT 80053) to $79.24 for a tissue exam by a pathologist (CPT88305). Significant geographic variation exists in the prices of in-network laboratory testing.
Out-of-network claims are highest in New York-New Jersey and Nassau-Suffolk. On a weighted average basis, median out-of-network reimbursement was 97.3% higher than in-network reimbursement. Excluding New York-New Jersey and Nassau-Suffolk (both outliers), the out-of-network reimbursement was 49.9% higher.
No Surprises Act
In-Network vs. Out-of-Network Rates — Pathology Services
Note:
Based on 2019 MarketScan Outpatient Services date limited to professional claims with pay (PAY) greater than 0 and (PROCMOD) not equal to ‘26’ or ‘TC’
88305: Tissue Exam By Pathologist
In-network 97.7% of claims; out-of-network 2.3%
In-network median allowed amount: $79.24; range $60.35 to $146.00
In-network median as % of Medicare: 106.0%
Out-of-network median allowed amount: $103.94; range $57.89 to $175.29
82306: Vitamin D
In-network 98.1% of claims; out-of-network 1.9%
In-network median allowed amount: $22.33; range $18.04 to $36.00
In-network median as % of Medicare: 75.4%
Out-of-network median allowed amount: $47.79; range $29.34 to $79.97
Analysis
The No Surprises Act is particularly focused on out-of-network claims. Providers and health plans can no longer bill patients beyond their in-network cost-sharing amount7. Collection of the differential will be subject to negotiation and, if unsuccessful, an Independent Dispute Resolution (IDR) process8.
The fundamental uncertainty involves payment for services beyond in-network contracted rates. A regression to the median contracted rate could result in a significant reduction in high-margin revenues. The magnitude of the financial reduction is also dependent on the number of out-of-network claims.
Financial risk is state- and MSA-dependent; 33 states have full- or partial-balance billing protections9. The state laws exclude enrollees of self-funded plans, which make up approximately 64% of the commercial population10. Median allowed amounts per CPT code vary significantly among MSAs. MSAs with the highest reimbursement often, but not always, have the highest percentage of out-of-network claims.
Alternative Analysis
The original methodology reflected whether an individual claim was paid as in-network or not. An alternative analysis was based on whether the provider of an individual service was a member of the payer’s network. The results were similar, with the exception that approximately 3.1% of claims were derived from out-of-network.
Litigation Update
On February 23, a federal judge challenged the independent dispute resolution (arbitration) process and its use of the median contracted price as the primary basis for a decision. Judge Kernodle of the U.S. District Court for the Eastern District of Texas ruled “that some parts of the interim final rule give too much power to insurers in the arbitration process and that HHS did not offer enough notice before it was implemented11.” An appeal from the U.S. Department of Health & Human Services (HHS) is expected; five other lawsuits are pending in the federal courts12.
The “hold” does not affect the entire No Surprises Act; it only affects the dispute resolution process affecting payers and providers.13 Due to Judge Kernodle’s decision, the median contracted price now represents a worst-case scenario with potential upside for providers. “Upside” still reflects a reduction in out-of-network prices but is above prior expectations based on median contracted rates.
Bottom Line
The No Surprises Act will affect the specialties with the greatest out-of-network reimbursement, including hospital-based pathology/laboratory services. Our analysis suggests a granular approach is necessary on a specialty and market basis to estimate the impact of the No Surprises Act. The major provider risk is a decline in prices to the median contracted rate should an Independent Dispute Resolution process be necessary. However, that risk is “on hold” pending litigation. Alternative positions are possible during the negotiation periods.
Footnotes:
1: Andes Robeznieks. “The No Surprises Act is in effect. What physicians need to know.” AMA; January 14, 2022 https://www.ama-assn.org/delivering-care/patient-support-advocacy/no-surprises-act-effect-what-physicians-need-know
2: Surprise Billing at A Glance. American Hospital Association (last visited February 10, 2022). https://www.aha.org/surprise-billing
3: The No Surprises Act’s Prohibitions on Balancing Billing. Centers for Medicare & Medicaid Services, Center for Consumer Information and Insurance Oversight (February 12, 2022). https://www.cms.gov/files/document/a274577-1a-training-1-balancing-billingfinal508.pdf
4: Ibid.
5: Ibid.
6: John Hargraves and Jean Fuglesten Biniek. “How common is out-of-network billing?” Health Care Cost Institute Inc. (November 21, 2019). https://healthcostinstitute.org/out-of-network-billing/how-common-is-out-of-network-billing
7: The No Surprises Act’s Prohibitions on Balancing Billing. Centers for Medicare & Medicaid Services, Center for Consumer Information and Insurance Oversight, page 15 (February 12, 2022). https://www.cms.gov/files/document/a274577-1a-training-1-balancing-billingfinal508.pdf
8: Ibid, page 16.
9: Maanasa Kona. “State Balance-Billing Protections.” The Commonwealth Fund (February 5, 2021). https://www.commonwealthfund.org/publications/maps-and-interactives/2021/feb/state-balance-billing-protections
10; Jenny Yang. “Percentage of U.S. workers covered by self-funded health insurance plans from 1999 to 2021.” Statista (November 11, 2021). https://www.statista.com/statistics/985324/self-funded-health-insurance-covered-workers/.
11: Jessie Hellmann and Alex Kacik. “Texas judge upends surprise billing law, for now.” Crain Communications, Inc. (February 24, 2022). https://www.modernhealthcare.com/legal/texas-judge-sides-docs-surprise-billing-lawsuit
12: Ibid.
13; Katie Keith. “Court Sets Aside Key Parts of No Surprises Act Rule.” Health Affairs (February 24, 2022) https://www.healthaffairs.org/do/10.1377/forefront.20220224.298748/
Related Insights
Related Information
Published
April 14, 2022
 Key Contacts
Key Contacts
Senior Managing Director
Senior Managing Director, Leader of Healthcare Business Transformation
Senior Managing Director
Downloads
Most Popular Insights
- Beyond Cost Metrics: Recognizing the True Value of Nuclear Energy
- Finally, Pundits Are Talking About Rising Consumer Loan Delinquencies
- A New Era of Medicaid Reform
- Turning Vision and Strategy Into Action: The Role of Operating Model Design
- The Hidden Risk for Data Centers That No One is Talking About


