- Accueil
- / Publications
- / Articles
- / Improving Patient Access: Three Strategic Initiatives for Healthcare Leaders
Improving Patient Access: Three Strategic Initiatives for Healthcare Leaders
-
novembre 22, 2024
-
In today’s rapidly evolving healthcare landscape, organizations are facing significant challenges in enhancing patient access. As patient expectations shift and demand for services increases, many organizations struggle to meet these needs, leading to longer wait times and decreased patient satisfaction.
This has created a pressing issue, as patients often experience frustration in securing timely appointments with providers. Consequently, these access challenges not only affect patient satisfaction but also pose risks to the operational efficiency, revenue leakage and overall success of ambulatory organizations. Prior to 2019, 81% of physicians described themselves as overextended or at full capacity.1 The post-pandemic era has only exacerbated these challenges.
Addressing these concerns through innovative technology solutions is essential for improving patient access and ensuring a positive patient experience. Below are high-level strategies that medical groups can leverage to mitigate these challenges. The article will explore each of these approaches in greater detail to provide deeper insight into their implementation and impact:
- Optimized Provider Templates: Streamlining and optimizing provider schedules can improve efficiency and increase patient access. This may involve adjusting appointment lengths, integrating more flexible scheduling options, and utilizing data to better match patient needs with provider availability.
- Referral Management Systems: Implementing or enhancing referral management systems can help manage patient flow and ensure that referrals are handled efficiently. This can reduce wait times and improve coordination between primary care and specialty providers.
- Self-Scheduling Capabilities: Providing patients with the ability to schedule their own appointments can improve access and patient satisfaction. Self-scheduling tools can also help manage demand by allowing patients to book appointments at their convenience, thereby reducing the administrative burden on staff.
Together, these solutions can help healthcare organizations better manage patient volume, improve access to care, and create a more responsive healthcare system. Read on for a closer look at how these strategies can be effectively implemented to maximize their impact.
Provider Template Optimization
Providing timely access to healthcare is one of the greatest predictors of patient satisfaction and is a key indicator of high-performing medical groups.2 As a result, new patient lag time is frequently used as the gold standard metric to assess patient access. New patient lag time is defined as the number of days between the scheduling date and appointment date, on average, across all appointments.3 The 2022 Survey of Physician Appointment Wait Times and Medicare and Medicaid Acceptance Rates reported it takes an average of 26 days to schedule a new patient physician appointment in 15 of the largest cities in the United States, up from 24.1 days in 2017, the last year the survey was conducted, and up from 21 days in 2004, when the survey was first conducted.4 Optimizing provider scheduling templates, through a combination of additional visits along with strategy for the right types of visits, is a highly effective tactic to reduce new patient lag time and increase patient satisfaction to meet organizational goals. Effective template strategies include:
Keeping templates simple — Striking the balance between provider preferences and template standardization has proven effective in maintaining sustainable patient access.5 Leveraging template strategy, built directly into the electronic health record (“EHR”), such as blocks with automated limits, is one way to control patient volume while increasing patient and provider scheduling flexibility. Incorporating flexibility into provider templates will enable adjustments for specific diagnoses and in-person versus telehealth appointments, urgent or same-day scheduling, and potentially extended hours where suitable.
Template strategy compliance — Schedulers who maintain template integrity significantly improve patient wait times and session lengths. Ad-hoc scheduling can increase patient wait times due to clinic inefficiencies and can lead to staff dissatisfaction. It is important to follow session limitations, block restrictions and overbook limits.6, 7
Self-scheduling functionality — Adoption of self-scheduling functionality in health care settings has lagged compared to other industries, despite patient expectations.8 Evidence has proven self-scheduling is advantageous to healthcare organizations: labor and operating costs are reduced, information transparency and provider punctuality increases, and patient satisfaction, accountability, loyalty and attendance improve.9 By removing the barriers of fixed scheduling staff and limited capacity of phone lines, patients’ scheduling experience is enhanced while the risk of open slots going unfilled on provider templates is reduced. The integration of automated, guided scheduling applications enhances the reliability of self-scheduling for patients, ensuring that each patient is matched with the right provider at the right time.
Review template key performance indicators (“KPIs”) — Key performance indicators are measurable values used to assess the effectiveness and success of an organization, department or individual in achieving specific objectives. Organizations should review templates biannually to identify scheduling strategies. Template optimization is not a “one and done” task. As provider protocols, technology and clinic support staff change, templates must adapt accordingly. Organizations should monitor the key scheduling and operational metrics below to prioritize template optimization opportunities:
- New patient lag time — number of days between the appointment scheduling date and new patient appointment date of service
- New patient appointment percentage — the total percentage of visits at which a patient is classified as new to the service offering
- Third next available — number of days (not counting non-worked days) until the third next available appointment
- Fill rate — the percentage of a provider's clinical volume filled with arrived patients
- Completed appointments — the number of scheduled clinic appointments completed
- No-shows — the percentage of non-canceled appointments that were either no-shows or late cancellations
- Time lost to no-shows — the total amount of time allocated to appointments that were marked as no-shows on a provider’s schedule
- Template utilization — the percentage of a provider's regular clinic volume filled with scheduled appointments, based on available appointment slots
- Error rates — the percentage of scheduling errors out of the total number of scheduled appointments over a specified period.
Referral Management
A high-functioning referral system reduces delays in patients obtaining medical care and services and offers functionality to monitor access to treatment for individuals.10 Optimizing the technology organizations have, or seeking innovative technology to enable non-manual processes, is key to becoming a high-functioning referral system and high-performing organization. Some organizations continue to utilize manual referral system management via email, phone, or even paper fax. This can cause extensive delays in patient access. Unless the patient is self-sufficient and savvy and can navigate the process themselves, there is risk of missing the referral altogether. There is also a greater possibility of error when required elements are not collected, thus increasing the potential for scheduling with the wrong provider and further hindering patient access.
Utilizing automated referrals within the EHR or with bolt-on applications* will expedite the patient’s access and optimize clinic operations. Beyond the ability to easily track automated referrals and reduce leakage, providers can speak to one another via a portal instead of playing phone tag. Additionally, medical records can be requested and received via the portal, and system rules will be followed that will minimize scheduling errors.
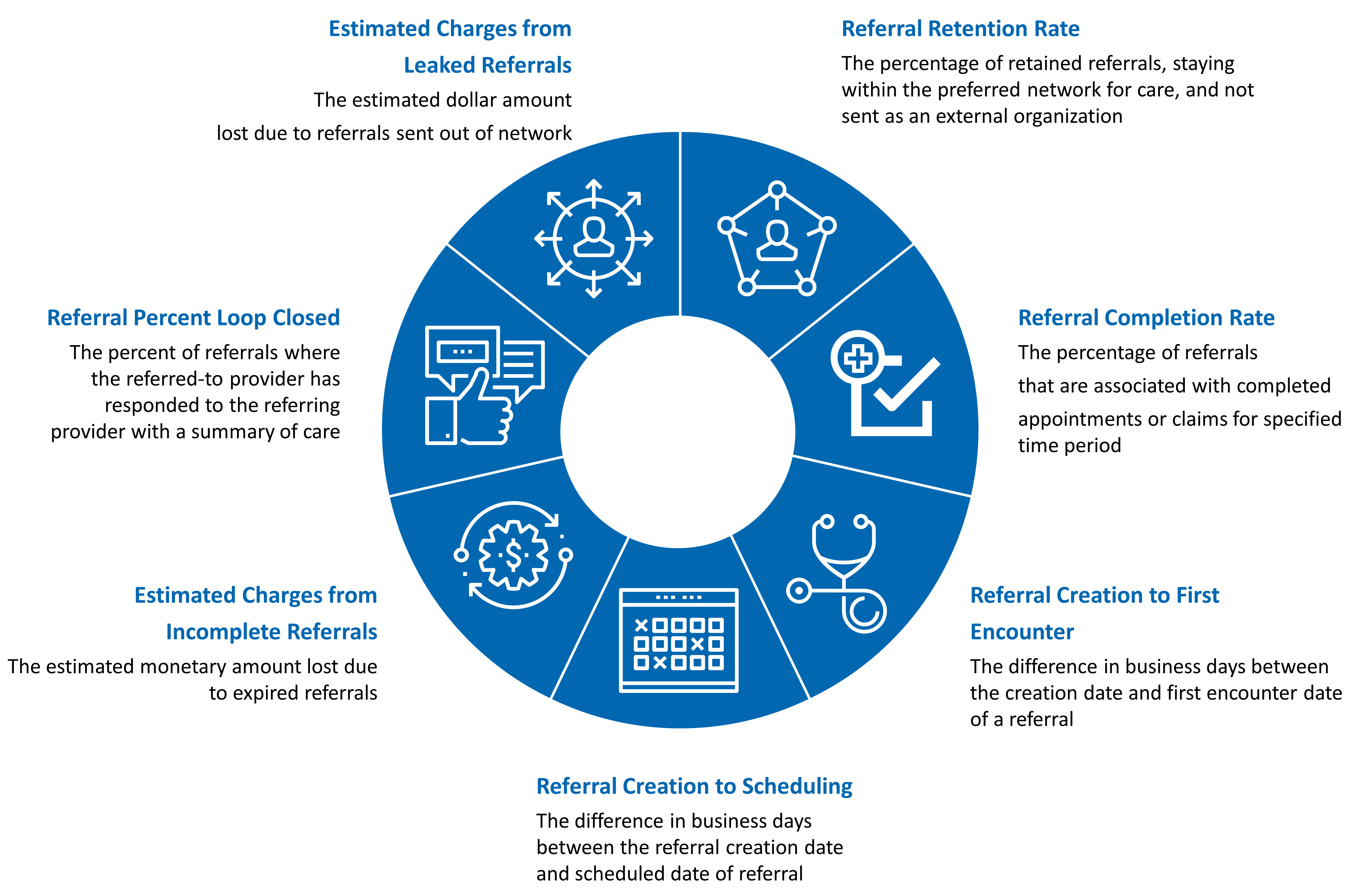
To monitor referral management and assess whether it effectively meets supply and demand while maximizing patient retention, organizations should track the following:
Self-Scheduling
Implementing self-scheduling systems significantly advances patient-centric care, efficiency and accessibility. This approach leverages technology to empower patients, streamline administrative processes and optimize healthcare provider workflows. Improved patient experience, reduced administrative burden and enhanced communication are some of the benefits of implementation. Bear in mind that, however, that implementing self-scheduling does require heavy planning and execution.
- Right Technology — The first thing to consider is the right technology; whether it is a current system capability or a bolt on system, the right technology will enhance the patient's experience and reduce the risk of scheduling errors.
- Thorough Assessment — Once technological decisions are made, a thorough assessment of current scheduling practices for specific areas must be undertaken with all appropriate stakeholders.
- Technical Build — The next steps after planning is completed are to build the technology into the system, test it and provide feedback, then training and support.
Items that must be considered during the planning phase include provisions for staff and patient adoption, patient privacy, system integration intricacies, and ongoing maintenance.
Implementing self-scheduling represents a major step toward enhancing patient engagement and operational efficiency. Not only does self-scheduling provide satisfaction to patients, but when used with automated guided scheduling, it is a game changer for medical practices as it ensures the right patient is seen by the right provider at the right time. By leveraging technology to automate and optimize appointment scheduling processes, healthcare providers can focus more on delivering quality care while empowering patients to manage their health actively. With careful planning, stakeholder engagement and ongoing technical support, organizations can successfully navigate the complexities and reap the benefits of self-scheduling to open patient access.
In a healthcare landscape marked by rising patient expectations and complex operational demands, adopting technology-driven strategies is not just advantageous — it’s essential. By adopting these innovative technology solutions, healthcare organizations can better manage patient volume, improve access to care and enhance overall service delivery. These approaches help align provider availability with patient needs and ultimately lead to a more efficient and responsive healthcare system.
Footnotes:
* A bolt-on application is additional software or a technology module that is added to an existing system to enhance its functionality. This approach allows organizations to integrate new capabilities or features without needing to replace their entire existing system.
1: “Survey of 20,000 U.S , Physicians Shows 80% of Doctors are Over-Extended or at Full Capacity, Demonst,” The Physicians Foundation (September 16, 2014).
2: Danial W. Barry, Trisha V. Melhado, Karen M. Chacko, Rita Shi-Ming Lee, John F. Steiner, and Jean S. Kutner, “Patient and Physician Perceptions of Timely Access to Care.” Journal of General Internal Medicine 21, no. 2 (February 2006): 130–33.
3: Ibid.
4: “Amn Healthcare Survey: Physician Appointment Wait Times up 8% from 2017, up 24% from 2004.” GlobeNewswire News Room (September 12, 2022).
5: Christine A. Sinsky, Hessam Bavafa, Richard G. Roberts, and John W. Beasley, “Standardization vs Customization: Finding the Right Balance.” The Annals of Family Medicine 19, no. 2 (March 2021): 171–77.
6: Michelle R. Hribar, Sarah Read-Brown, Leah Reznick, and Michael F. Chiang, “Evaluating and Improving an Outpatient Clinic Scheduling Template Using Secondary Electronic Health Record Data.” AMIA Annu Symp Proc (April 16, 2018), 921–29. PMID: 29854159.
7: Ibid.
8: Elizabeth Woodcock, “Barriers to and Facilitators of Automated Patient Self-scheduling for Health Care Organizations: Scoping Review,” J Med Internet Res 24, no. 1 (November 1, 2022), DOI: 10.2196/28323.
9: Ibid.
10: Ali Akbari-Sari, Maryam Seyed-Nezhad, and Batoul Ahmadi, “Factors Affecting the Successful Implementation of the Referral System: A Scoping Review.” Journal of Family Medicine and Primary Care 10, no. 12 (2021): 4364.
Date
novembre 22, 2024
 Contacts
Contacts
Managing Director
Senior Director
Director
Director
Most Popular Insights
- Beyond Cost Metrics: Recognizing the True Value of Nuclear Energy
- Finally, Pundits Are Talking About Rising Consumer Loan Delinquencies
- A New Era of Medicaid Reform
- Turning Vision and Strategy Into Action: The Role of Operating Model Design
- The Hidden Risk for Data Centers That No One is Talking About