The Future of Care Delivery
Improving Outpatient Experience by Integrating Journey Maps and Digital Health
-
September 28, 2022
DownloadsDownload Article
-
In this article we provide an example of an outpatient journey map, discuss patient engagement and self-management, and highlight the growing importance of a personalized digital experience.
The Institute for Healthcare Improvement’s framework to optimize health system performance includes the “Triple Aim”: improving the patient experience of care (including quality and satisfaction); improving the health of populations; and reducing the per capita cost of health care.1 The Agency for Healthcare Research and Quality (“AHRQ”) defines patient experience as encompassing “the range of interactions that patients have with the healthcare system, including their care from health plans, and from doctors, nurses, and staff in hospitals, physician practices, and other healthcare facilities.”2 As technology evolves and patients pay an increasing proportion of out-of-pocket costs, their experiences increasingly parallel those of retail consumers.
Patient journey maps depict the path taken by patients as they navigate the healthcare system. Insights are generated, expectations defined, processes assessed, and steps taken to enhance the patient experience. More specifically, journey maps have been used to increase customer satisfaction, develop new products or services, identify gaps in communication touchpoints and prioritize customer-centric initiatives.3
Patient engagement and self-management support essential to the outpatient journey
Patient engagement has been defined “as a concept that combines a patient’s knowledge, skills, ability, and willingness to manage his own health and care with interventions designed to increase activation and promote positive patient behavior.”4 Patient engagement is critical, as behavioral (lifestyle) patterns and social circumstances represent 40 percent and 15 percent, respectively, of the contributors to premature death.5
Patient engagement requires self-management support, defined by the Institute of Medicine (“US”) as “the systematic provision of education and supportive interventions by health care staff to increase patients’ skills and confidence in managing their health problems, including regular assessment of progress and problems, goal setting, and problem-solving support.”6
According to the AHRQ, patients with chronic illnesses may be asked to:
- “Closely monitor symptoms.”
- Respond with appropriate actions (adjust medications, initiate call to a health care coach, schedule a doctor visit) when symptom levels indicate a problem.
- Make major lifestyle changes (e.g., stop smoking, reduce alcohol consumption, modify diet, lose weight, and increase exercise).
- Adhere to medication regimens, some of which are inconvenient or produce side effects.
- Make office visits for lab tests, physical exams, and clinician consultations.”7
The ability of a patient to self-manage depends on many factors, including their knowledge; psychosocial mediators such as self-efficacy, attitudes, health beliefs, mood, motivation, and coping skills; lifestyle behaviors; and degree of social support.
Knowledge alone is insufficient to result in significant behavior change; however, it is integral to the process of change.8 Knowledge attainment requires health literacy; inadequate literacy is independently associated with worse outcomes and higher rates of hospitalization and emergency services utilization.9 Nearly half of the adult U.S. population has difficulty understanding and using health information, that is, the ability to understand instructions on prescription drug bottles, appointment slips, medical education brochures, doctor’s directions and consent forms, and the ability to negotiate complex health care systems.10
Customer service and communications as determinants of satisfaction
In 2012, The Physicians Foundation conducted a comprehensive survey among consumers (n=1,800) on their satisfaction levels with their primary care physician.11 Satisfaction was high; customer service, communications and treatment processes were its primary drivers.12
Nearly 10 years later, Redpoint Global highlighted its survey results (n=1,000) with the following headline: “Healthcare Consumers Weigh In: Personalized Experiences are a Must.”13 “[A] majority of respondents (80 percent) said that they prefer to use digital channels (online messaging, virtual appointment, text, etc.) to communicate with healthcare providers and brands at least some of the time;” “66 percent said that selecting a provider was dependent on the provider’s ability to communicate to them in a timely and consistent manner;” and “(60 percent) said that they would choose a provider based on how well the provider understands them, beyond basic patient data, so that the experience is relevant and personalized.”14 The results are not dissimilar from The Physicians Foundation survey of 2012, with the exception of digital enablement.
Patients were very or extremely satisfied with their primary care physician (79%) in 2012
Reasons for Satisfaction
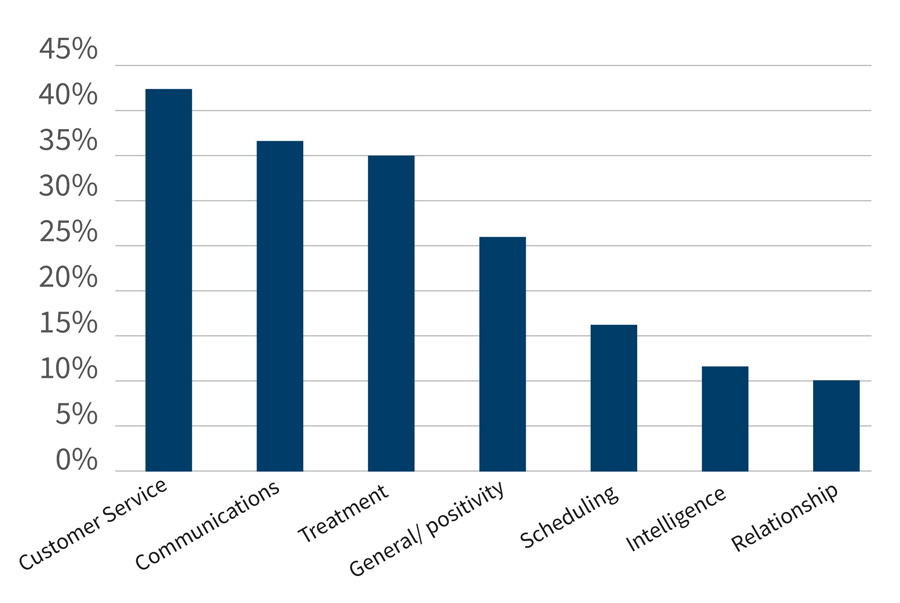
Source: The Physicians Foundation (October 17, 2012).
Patient segmentation: Not all patients are alike
“Personas” can be used as the foundation for healthcare journey maps: “Personas are fictional [composite] characters, which you create based upon your research to represent the different user types that might use your service, product, site, or brand in a similar way. Creating personas will help you understand your users’ needs, experiences, behaviors and goals.”15 Different people (personas) have different needs and expectations.
User experience (UX) design is about designing the ideal experience of using a service or product.16 Seven factors influence the user experience: useful, usable, findable, credible, desirable, accessible, and valuable.17 It is a complex subject requiring expert assistance.
Shifting focus from “push” to “pull”
Recognition of behavioral change as a complex process requires a fundamental paradigm shift in the provider approach to patient interaction from “push” to “pull.” Unidirectional and infrequent contacts must be replaced with bidirectional, frequent and timely contacts focused on developing self- management and caregiver support skills. The availability of consumer portals, combined with the advent of multi-channel digital media and enabling technology, facilitates the generation of a lower-cost “pull” approach to “whole person” care delivery. It takes an average of 66 days to form a new habit, with a range of 18 to 254 days.18
Digital Health and Medicare: An untapped and challenging opportunity
The U.S. population >65 years old is projected to increase in 2020-2030 from 56.1 million to 73.1 million, or from 16.5% to 20.3% of the total population.19 The compound annual growth rate is highest for the 75-84 age cohort (4.4%), followed by the >85 cohort (3.1%) and the 65-74 cohort (1.7%); population growth in the < 65 age group is minimal at 0.2%.20 Medicare spending is forecast to increase from $0.8 trillion in 2020 to $1.7 trillion in 2030, reflecting a compound annual growth rate of 7.2%.21 Per capita expenditures increase with age.22 The costliest 10% of beneficiaries account for 60% of spending; the costliest 25% account for 84% of spending.23
Higher spending among the aged reflects an increase in co-morbidities and/or worsening condition severity. Serious chronic conditions are complicated by the presence of depression in 25%-33% of patients and activity limitations.24,25 End-of-life spending accounts for 25.1% of Medicare spending and exceeds $100,000 per patient.26 Heart disease and cancer are the leading causes of death, followed by COVID-19, unintentional injuries (accidents), stroke, COPD, Alzheimer’s disease, and diabetes.27
Aging population associated with rising chronic disease burden
Aging Baby Boomers, 2010-2030
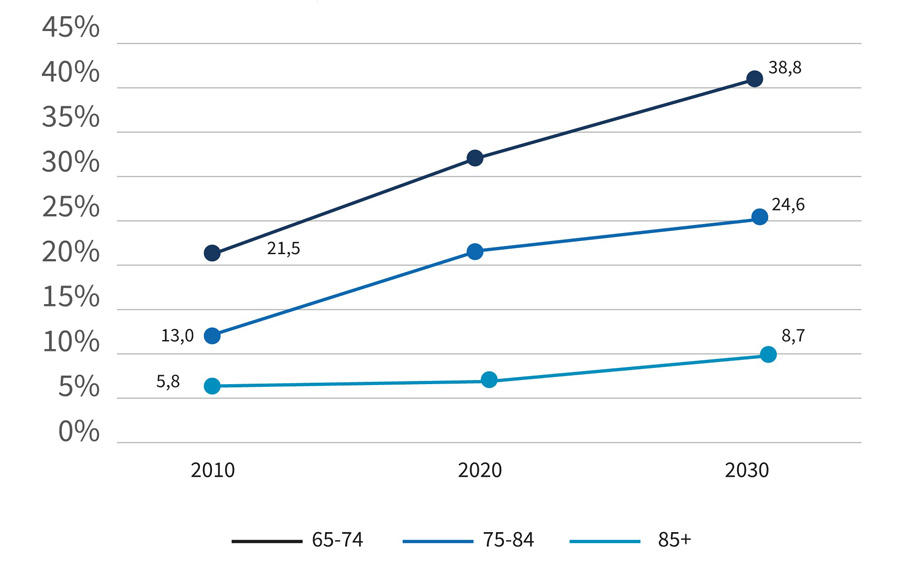
Source: U.S. Census Bureau; Medicare Chronic Condition Warehouse (2017).
Personalized outpatient journey map identifying opportunities for intervention
The patient journey involves a 68-year-old obese male with diabetes, hypertension and depression. The patient has recovered from surgery and notices his blood glucose is elevated and he has an increased frequency of urination. An appointment is scheduled with his physician who confirms that his diabetes is “out-of-control.” The patient medications are altered. He is enrolled in the health system’s digital health program for patients with chronic diseases. He is also provided access to a psychologist. It is important to “capture the interplay among [the] customer, care teams, technology, and data.”28
Enabling digital tools have been developed for each of these steps. Successful delivery system redesign requires focusing on secondary prevention (early detection and intervention) and tertiary prevention (treating established disease to prevent deterioration), closing gaps in care, managing care transitions (e.g., from hospital to home), treating behavioral health issues, facilitating self-management and, if appropriate, offering palliative care. Home-based care is preferential to hospitals and skilled nursing facilities. Digital transformation, as exemplified by telehealth, enhances timely access and intervention.
Varying chronic diseases affecting the >65 population
Chronic Disease Prevalence in Medicare FFS Beneficiaries >65
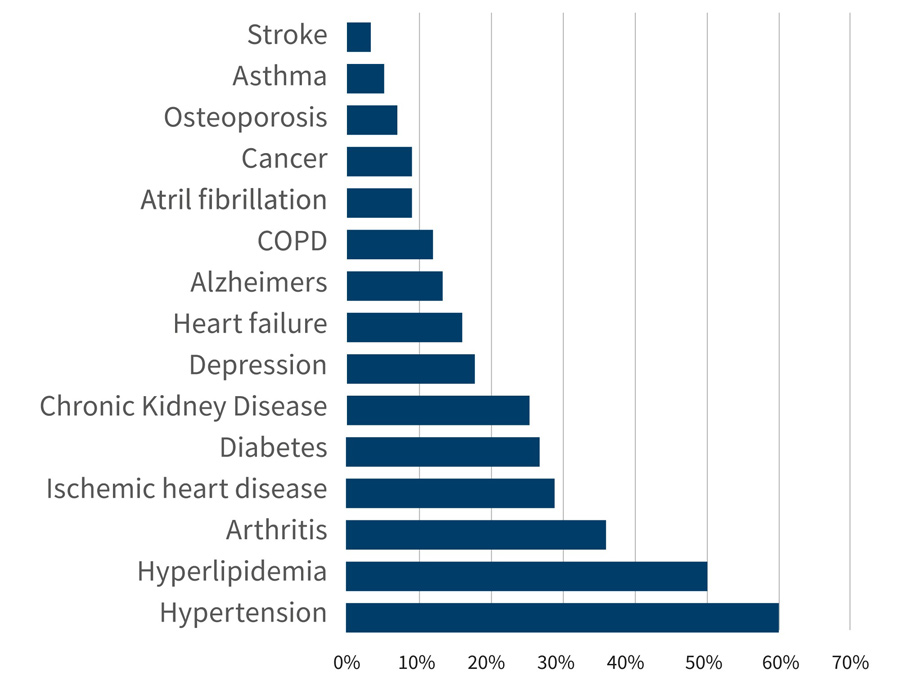
Source: U.S. Census Bureau; Medicare Chronic Condition Warehouse (2017).
Chronic care patient journey optimization requires enhanced self-management
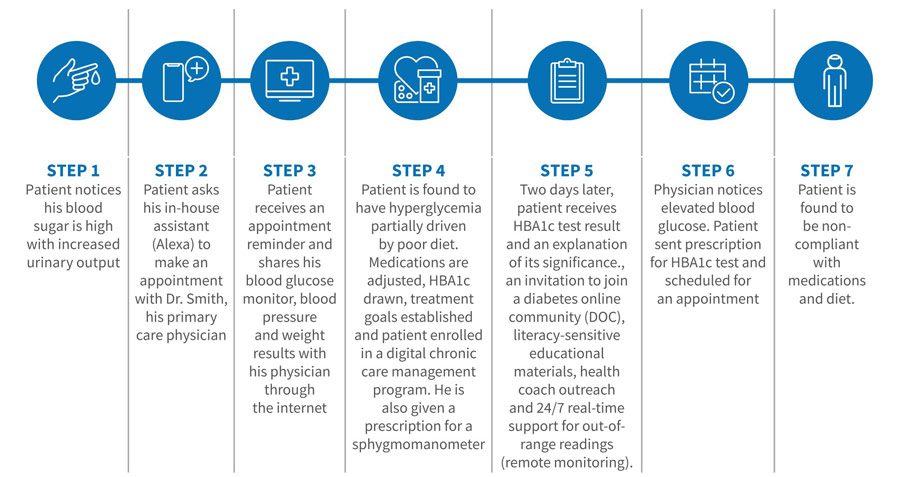
Source: FTI Consulting
Mature contact centers provide a single point of contact for customers, improve access to all service offerings and enhance the customer experience. An omnichannel, unified contact center approach involves voice, mobile, web, video, e-mail, social media and chat bot technologies. Patients demand self-service as well as other options to quickly access the services they need. Emerging technologies include the growing use of chat bots, voice analytics (key words, sentiment, etc.) and automated clinical decision trees to further support this self-service experience.
Remote monitoring technologies are currently being used to monitor vital signs (heart rate, respiratory rate, temperature and blood pressure), weight, blood glucose levels (glucometer), blood oxygen levels (pulse oximetry), atrial fibrillation, activity (steps taken, distance traveled, calories) and sleep.29 Emerging technologies target seizure disorders, neuromuscular conditions, COPD and pneumonia, and other conditions.30 These technologies enable care-at-home.
Digital health programs exist for diabetes and prediabetes, hypertension, heart failure, behavioral health and other chronic conditions.31 Glucometers, blood pressure cuffs and weight scales connect to a central station for the reporting of out-of-range results.32 Health goals are established, personalized action plans and tips provided, nudges generated, and health coaches made available to create an integrated healthcare experience.
The presence of a mental health disorder in patients with chronic disease has been associated with higher costs, hospitalization rates and emergency department visits.33 A study completed in Canada found three-year mean costs of $34,690 for patients with chronic disease and depression as compared to $20,210 for those with chronic disease alone.34
A plethora of digital mental health platforms have been introduced, though relatively few targeting co-morbid chronic disease. Telehealth accounts for 35% of mental health and substance use disorder outpatient visits, a figure far exceeding the 5% reported for all other out patient visits.35
Medication nonadherence is exceedingly common, affecting 40% to 50% of patients with chronic disease.36 Noncompliance may result from patient-related barriers such as low perceived necessity (especially when asymptomatic) and lack of understanding of the proper use, purpose and benefit of therapy, and from treatment-related barriers including complexity of treatment, side effects, loss or lack of drug response and high out-of-pocket costs.37 Changing patient behavior is difficult but necessary to improve adherence.
A study from 2017 “found no conclusive evidence of improved medication adherence using digital health interventions such as interactive voice response (IVR), short messaging service (SMS) text messaging, telemonitoring, and interactive software technology.”38 Digital containers to organize pills with apps to generate reminders are currently available.39
Bottom line
Journey maps facilitate visualization of care pathways from the patient’s perspective. Digital tools, in conjunction with journey maps, can be used to enhance the patient experience. A sense of urgency is required, as patients are increasingly willing to change providers based on their service experience, inclusive of access and communications.40
Footnotes:
1: The IHI Triple Aim. Institute for Healthcare Improvement (last visited May 15, 2022). https://www.ihi.org/Engage/Initiatives/TripleAim/Pages/default.aspx.
2: What is Patient Experience? Agency for Healthcare Research and Quality (page last reviewed May 16, 2022). https://www.ahrq.gov/cahps/about-cahps/patient-experience/index.html.
3: The State of Mapping the Customer Journey. Hanover Research (last visited May 31, 2022). https://cdn2.hubspot.net/hubfs/3409306/The-State-of-Customer-Journey-Mapping_final.pdf.
4: Michelle Ronan Noteboom. What does ‘patient engagement’ really mean? Healthcare IT News (May 1, 2015). https://www.healthcareitnews.com/news/what-does-patient-engagement-really-mean.
5: Stephen A. Schroeder, M.D. We Can Do Better – Improving the Health of the American People. NEJM 2007; 357: 1221-1228. September 20, 2007. https://www.nejm.org/doi/full/10.1056/nejmsa073350.
6: Institute of Medicine (US) Committee on the Crossing the Quality Chasm: Next Steps Toward a New Health Care System; Adams K, Greiner AC, Corrigan JM, editors. The 1st Annual Crossing the Quality Chasm Summit: A Focus on Communities. Washington (DC): National Academies Press (US); 2004. Chapter 5, Patient Self-Management Support. Available from: https://www.ncbi.nlm.nih.gov/books/NBK215507/#:~:text=Self%2Dmanagement%20support%20is%20defined,%2C%20and%20problem%2Dsolving%20support.
7: What is the State of Patient Self-Management Support Programs? An Evaluation. Agency for Healthcare Research and Quality (page last reviewed October 2014). https://www.ahrq.gov/research/findings/final-reports/selfmgmt/selfmgmt3.html.
8: Jennifer La Guardia. Why knowledge alone doesn’t create behavior change. Omada Health (July 10, 2019) https://www.omadahealth.com/news/why-knowledge-alone-doesnt-create-behavior-change
9: An Introduction to Health Literacy: What Is Health Literacy? National Library of Medicine (page last updated December 17, 2021). https://nnlm.gov/guides/intro-health-literacy.
10: Institute of Medicine (US) Committee on Health Literacy; Nielsen-Bohlman L, Panzer AM, Kindig DA, editors. Health Literacy: A Prescription to End Confusion. Abstract. Washington (DC): National Academies Press (U.S.); (2004). Executive Summary. Available from: https://www.ncbi.nlm.nih.gov/books/NBK216029/.
11: New Survey Finds Nearly 80 Percent of U.S. Patients “Extremely or Very Satisfied” With Primary Care Physician Visits. The Physicians Foundation (October 17, 2012). https://physiciansfoundation.org/physician-and-patient-surveys/consumer-survey/.
12: Ibid.
13: John Nash. Healthcare Consumers Weigh In: Personalized Experiences are a Must. Redpoint Blog (December 7, 2021). https://www.redpointglobal.com/blog/healthcare-consumers-weigh-in-personalized-experiences-are-a-deal-breaker/.
14: Ibid.
15: Rikke Friis Dam and Teo Yu Siang. Personas - A Simple Introduction. (last visited May 18, 2022). https://www.interaction-design.org/literature/article/personas-why-and-how-you-should-use-them.
16: The Basics of User Experience Design. Interaction Design Foundation (last visited May 27, 2022). https://www.interaction-design.org/ebook
17: Ibid.
18: James Clear. How Long Does It Actually Take to Form a New Habit? (Backed by Science). James Clear, hosting by LiquidWeb (last visited June 9, 2022). https://jamesclear.com/new-habit.
19: 2017 National Population Projections Tables: Main Series, Detailed Age Group and Sex Composition of the Population. Projections for the United States, 2017-2060; Main Series, Table 3 (2017). https://www.census.gov/data/tables/2017/demo/popproj/2017-summary-tables.html.
20: Ibid.
21: Centers for Medicare & Medicaid Services, National Health Expenditure Data, Projected; Table 17 (page last modified April 27, 2022). https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsProjected.
22: A Data Book: Healthcare Spending and the Medicare Program. MedPAC (July 2021). https://www.medpac.gov/wp-content/uploads/import_data/scrape_files/docs/default-source/data-book/july2021_medpac_databook_sec.pdf.
23: Ibid.
24: Steve Melek and Doug Norris, Chronic conditions and comorbid psychological disorders. Milliman (July 2008). https://www.cbhc.org/wp-content/uploads/2015/11/chronic-conditions-and-comorbid-RR07-01-08.pdf.
25: Jennifer Casarella, MD. Dealing With Chronic Illnesses and Depression. WebMD (September 27, 2020). https://www.webmd.com/depression/guide/chronic-illnesses-depression#1.
26: Gerald F. Riley and James D. Lubitz. Long-Term Trends in Medicare Payments in the Last Year of Life. Health Serv Res. 2010;45(2):565–576. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2838161/.
27: Leading Causes of Death. National Center for Health Statistics, Centers for Disease Control and Prevention (last visited May 27, 2022). https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm.
28: Preparing for Healthcare’s Next Act: A Guide to Shaping the Customer Experience. Hero Digital (2020). https://herodigital.com/wp-content/uploads/2020/11/Hero-Digital_Healthcare-Next-Act_11.18.2020.pdf.
29: Digital Health Trends 2021: Innovation, Evidence, Regulation, and Adoption. IQVIA Institute for Human Data Science (July 22, 2021). https://www.iqvia.com/insights/the-iqvia-institute/reports/digital-health-trends-2021.
30: Ibid.
31: Powering a chronic care revolution. Welldoc (last visited May 15, 2022). https://www.welldoc.com/solutions/chronic-care-management-platform/.
32: Take charge of your health. Livongo (last visited May 15, 2022). https://www.livongo.com/.
33: Barbora Sporinova, MD, Braden Manns, MD, Marcello Tonelli, MD, et al. Association of Mental Health Disorders With Health Care Utilization and Costs Among Adults With Chronic Disease. JAMA Network (2019; 2(8)). https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2748662.
34: Ibid.
35: Justin Lo, Mathew Rae, Krutika Amin, Cynthia Cox, Nirmita Panchal, Benjamin F. Miller. Telehealth Has Played an Outsized Role Meeting Mental Health Needs During the COVID-19 Pandemic. Kaiser Family Foundation (March 15, 2022). https://www.kff.org/coronavirus-covid-19/issue-brief/telehealth-has-played-an-outsized-role-meeting-mental-health-needs-during-the-covid-19-pandemic/.
36: Fred Kleinsinger. The Unmet Challenge of Medication Nonadherence. The Permanente Journal. (2018; 22: 18-33). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6045499/.
37: Ibid.
38: Cheryl Moseley Conway and Teresa J. Kelechi. Digital Health for Medication Adherence in Adult Diabetes or Hypertension: An Integrative Review. JMIR Diabetes 2017;2(2): e20. https://diabetes.jmir.org/2017/2/e20.
39: Never Miss Your Pills Again! elliegrid (last visited May 18, 2022). https://elliegrid.com/.
40: Todd Shryock. 69% of patients would switch providers for better services. Medical Economics (February 15, 2022). https://www.medicaleconomics.com/view/69-of-patients-would-switch-providers-for-better-services.
Related Insights
Related Information
Published
September 28, 2022
 Key Contacts
Key Contacts
Managing Director
Downloads
Most Popular Insights
- Beyond Cost Metrics: Recognizing the True Value of Nuclear Energy
- Finally, Pundits Are Talking About Rising Consumer Loan Delinquencies
- A New Era of Medicaid Reform
- Turning Vision and Strategy Into Action: The Role of Operating Model Design
- The Hidden Risk for Data Centers That No One is Talking About


