A Playbook for Hospital Stabilization and Recovery
Clinical, Financial and Operational Pathways to Resilience
-
November 14, 2025
-
The end of pandemic-era funding, along with rising labor and operating costs, has increased pressure on health systems and the communities they serve. Many U.S. hospitals are now facing significant — and in some cases terminal — financial challenges.
These challenges are sparking a period of transformation, as health systems reimagine how to sustain care delivery, workforce stability and community partnerships. While state-directed payments can help bridge near-term needs, the broader opportunity lies in building more resilient, adaptive models of care.
Drawing on years of experience working alongside state agencies, health systems and hospital operators facing these challenges, our experts have identified common patterns that separate short-term fixes from lasting recovery. This playbook combines core stabilization steps with broader recovery enablers to help organizations protect access to care, preserve community value and restore resilience.
Causes of Distress
Diagnosing the root causes of distress is essential to preventing hospital closures that threaten not only access to care but also the economic and social well-being of the communities they serve. Safety net, community, rural and for-profit facilities are all at heightened risk.
Hospital distress rarely stems from a single issue. Instead, pressures accumulate, sometimes over a prolonged period and in ways that are difficult to pinpoint, often leading to systemic struggles across the organization. These pressures fall into four broad, interrelated categories of distress:
- Financial: inability to generate consistent cash flow to fund daily operations, maintain infrastructure and invest in critical needs
- Operational: inadequate staffing, capacity and service offerings that limit access, extend wait times and strain quality and consumer satisfaction
- Regulatory and policy: gaps in meeting compliance standards that erode community trust, reduce reimbursement and impact patient outcomes
- Market dynamics: ongoing pressure from evolving reimbursement models, rising labor and technology costs and increased competition, leading to patient leakage
Playbook for Hospital Stabilization and Recovery
Our experts have proposed a playbook with practical elements for assessing risk, prioritizing interventions and guiding hospitals toward stability. Effective stabilization goes beyond liquidity; it preserves access to care, protects patients and sustains the hospitals that anchor their communities.
Typical Pathway to Stability
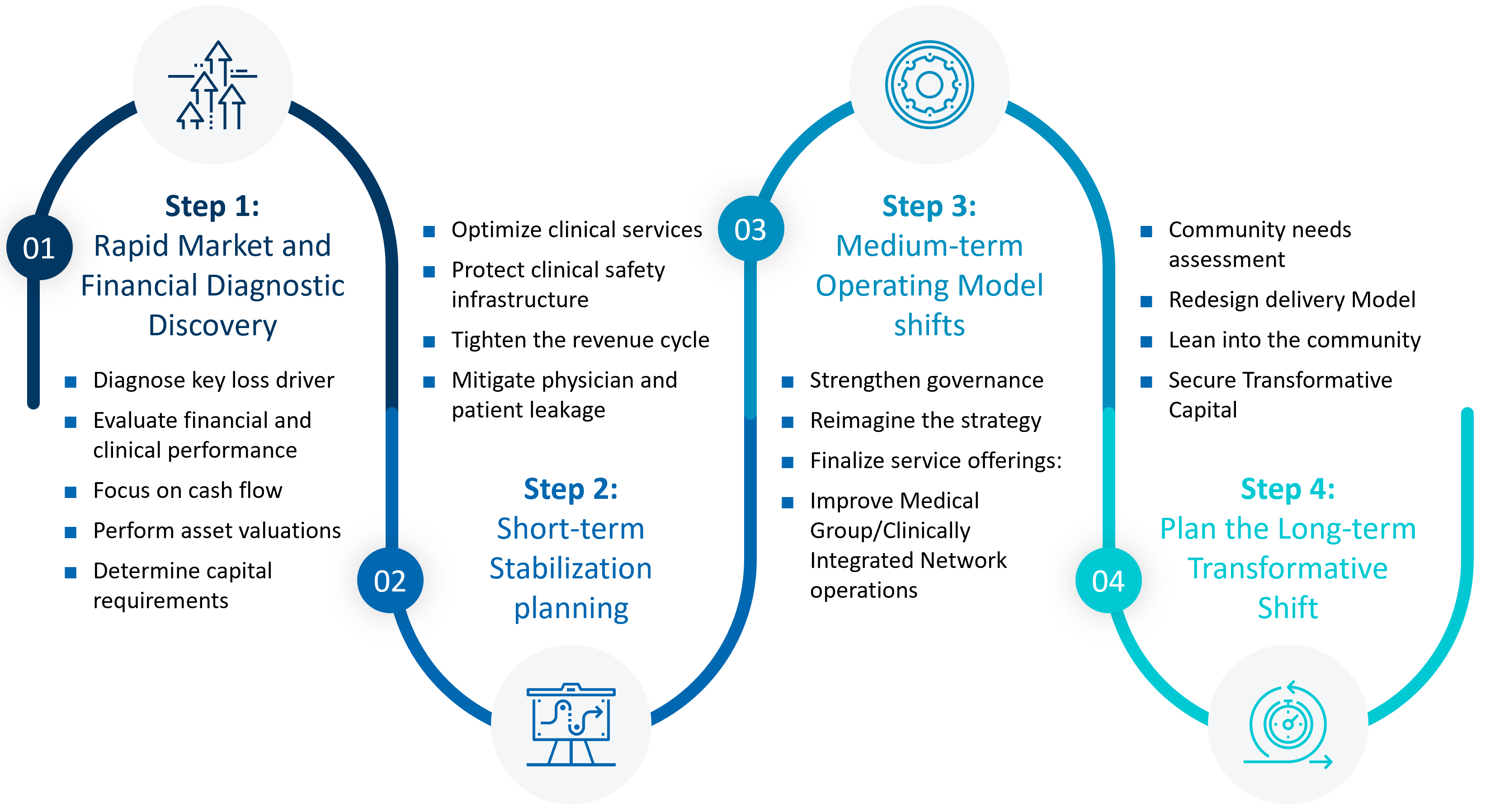
Source: FTI Consulting
Step 1: Rapid Market and Financial Diagnostic Discovery
Whether an organization is in a decline or in a crisis, the first call to action is to determine the root causes of the pressure it is facing through due diligence.
- Diagnose key loss drivers: Identify which services and cost centers require the most investments to enable resource alignment and improve operational focus.
- Evaluate financial and clinical performance: Assess care quality and safety metrics alongside financial indicators to detect high-risk service lines early and connect operational issues to patient outcomes.
- Focus on cash flow: Identify immediate drains, develop forecasts and, if needed, implement daily management of working capital and vendor negotiations to restore liquidity.
- Perform asset valuations: Assess all non-core assets to identify opportunities and strengthen the balance sheet.
- Determine capital requirements: Clarify funding needed for mandatory maintenance and strategic investments, ensuring debt servicing capacity and strategic alignment of all future capital deployment.
Step 2: Short-Term Stabilization Planning
Immediate interventions should focus on restoring operational stability and protecting core services.
- Optimize clinical services: Rapidly refine service lines and medical group operations to reduce complexity, eliminate inefficiencies and focus resources on profitable, high-demand care.
- Protect clinical safety infrastructure: Ensure safety programs, daily huddles, event reporting and leadership visibility continue even during financial compression to maintain focus on patient safety and quality outcomes.
- Tighten the revenue cycle: Implement immediate changes to billing practices, coding accuracy and collections efficiency to quickly increase cash realization and reduce preventable denials.
- Mitigate physician and patient leakage: Investigate drivers of patient attrition and physician turnover, focusing on critical workforce retention strategies to protect core revenue.
At this stage it is important to begin an open dialogue with your leaders, bringing your vision to them, helping to reduce anxiety and gain trust.
Step 3: Medium-Term Operating Model Shifts
Once short-term stability is achieved, attention must turn to strategic and operational redesign.
- Strengthen governance: Establish clear, disciplined decision-making structures across leadership and the board to ensure rapid consensus and accountability for strategic shifts. Embed physician leadership within this governance model to align clinical decision-making with fiscal accountability and operational priorities.
- Reimagine the strategy: Develop and gain consensus on a sustainable future operating model, clearly outlining the organization’s destination and value proposition.
- Finalize service offerings: Determine the definitive scope of clinical services, encompassing both core inpatient operations and a focused, growth-oriented ambulatory network.
- Improve medical group/clinically integrated network operations: Quickly identify optimization tactics in physician practices support, productivity and scheduling to increase revenue and reduce investment.
Step 4: Plan the Long-Term Transformative Shift
- Community needs assessment: Conduct a review to confirm the essential health services and capabilities the community requires for the long term.
- Redesign delivery model: Develop clinical and operational processes to closely match the confirmed community reality, ensuring services are accessible, efficient and appropriate.
- Lean into the community: Actively engage with foundations, like-minded non-profits and strategic partners to secure external resources and shared commitment to the hospital’s future.
- Secure transformative capital: Identify the specific funding required to evolve, utilizing strategic opportunities like joint ventures, ambulatory surgery centers, and value-based care repositioning.
Organizing for the Future
Beyond immediate stabilization, hospitals must also navigate the broader set of factors that enable or extend recovery. These pathways and enablers help sustain progress and create conditions for long-term viability.
Strategic and Structural Options
When underlying challenges cannot be resolved through operational measures alone, organizations should evaluate structural options that preserve access and community value. True stabilization succeeds when clinical integrity and financial discipline move in tandem; neither is likely to succeed in isolation. In addition to supporting operational restructuring, over the medium term, hospitals can:
- Pursue strategic partnerships: Evaluate mergers, affiliations or joint ventures to enhance organizational scale, improve access to capital and drive service line diversification.
- Evaluate aggressive options: Determine if the depth of impairment requires using bankruptcy as a formal tool to temporarily stabilize cash flow, buy time or help facilitate a structured sale or merger.
Communication and Stakeholder Engagement
Across all phases of transformation, communications and stakeholder engagement are critical to success.
- Establish clear leadership and coordination: Identify key decision-makers early and align on who drafts, reviews and approves communications to enable rapid, consistent responses.
- Engage stakeholders early and often: Communicate proactively with employees, clinicians, board members, community leaders and government partners to build trust and reduce disruption.
- Communicate with empathy and transparency: Provide timely, factual updates, anticipate media attention and correct misinformation quickly to maintain credibility and public confidence.
The Role of the Public Sector and Policymakers
Hospital recovery rarely happens in isolation. State and federal partners play a critical role in shaping the environment in which stabilization can succeed.
- Leverage available programs and support: Waivers from the Center for Medicare & Medicaid Services, state-directed payments and rural stabilization funds can extend the runway for recovery.
- Coordinate with regulators early: Transparent dialogue builds trust and reduces the risk of compliance surprises.
- Align financial plans with policy priorities: Linking recovery efforts to access, workforce and equity goals can unlock collaboration and support.
Healthcare Quarter
in Review
Read Now
The Bottom Line
Stabilizing distressed hospitals isn’t just about keeping the lights on. It’s about preserving the backbone of community health and economic vitality. Ultimately, sustainable recovery depends on proper diagnostics and acceptance of a new operational reality that aligns mission with a financial plan and details the steps of execution.
State leaders, hospital boards and local partners that align around data-driven decision-making, community partnerships, discipline and proactive governance can position a facility for renewal. Together, they can build sustainable healthcare networks that strengthen both community well-being and resilience.
Related Insights
Related Information
Published
November 14, 2025
 Key Contacts
Key Contacts
Senior Managing Director, Head of Americas Healthcare & Life Sciences
Senior Managing Director
Senior Managing Director
Shaun Rangappa, M.D., M.S.H.A.
Senior Managing Director
Senior Managing Director
Most Popular Insights
- Beyond Cost Metrics: Recognizing the True Value of Nuclear Energy
- Finally, Pundits Are Talking About Rising Consumer Loan Delinquencies
- A New Era of Medicaid Reform
- Turning Vision and Strategy Into Action: The Role of Operating Model Design
- The Hidden Risk for Data Centers That No One is Talking About


